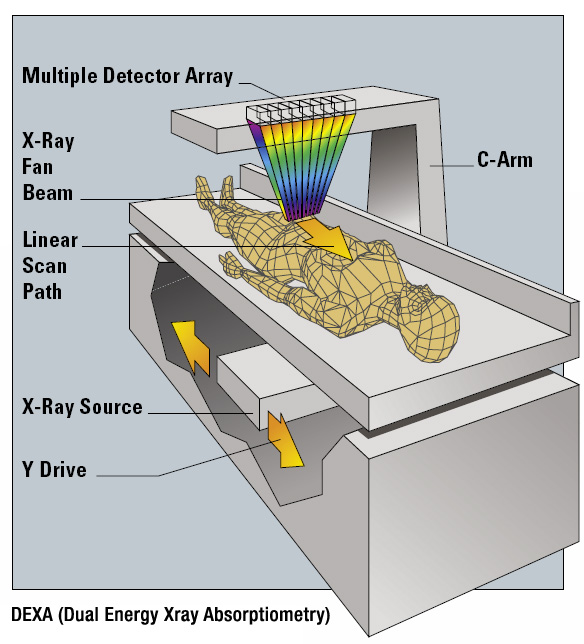
In the first five parts of this series, I discussed various 2-compartment models of estimating body composition. These models divide the body into fat and fat-free mass. Now let's talk about a common 3-compartment model: dual-energy x-ray absorptiometry (DEXA).
DEXA
DEXA, once used for determining bone density, evolved into a technique for also estimating body composition. DEXA represents a 3-compartment model for estimating body composition, because it can divide the body into 3 compartments: fat, bone mineral, and all other fat-free mass that does not include bone. Thus, unlike 2-compartment models, DEXA is not subject to errors caused by variations in bone density among different ethnicities. However, there are other sources of error which I will discuss in this article.
DEXA offers a number of advantages. Improved technology has dramatically decreased scan times (years ago, a DEXA scan would take 20-25 minutes; now scans can take 5-10 minutes), so the method is convenient and non-invasive. DEXA can provide bone density estimates, and can provide regional estimates of body composition (meaning it can estimate the body composition of individual parts of your body). DEXA works by measuring your body's absorbance of x-rays at two different energies. Fat, bone mineral, and fat-free soft tissue have different absorption properties. Thus, we can get estimates of your body composition by scanning your entire body.
DEXA Sources of Error
Like all other body fat estimation techniques, DEXA has numerous sources of error. There can be inconsistent results between different machines from different manufacturers, and even different results between machines from the same manufacturer. Software upgrades can change the algorithms that the device uses to calculate body composition. Different hardware and software configurations can result in different interpolations of soft tissue over bone, and different treatment of pixels of which a small portion is bone. The type of X-ray beam (fan beam or pencil beam) can also be a source of error; DEXA machines with fan beams can suffer from beam magnification (also known as parallax error). A final source of error is the same error that all 2-compartment models also have: the hydration of fat-free mass. In fact, a 5% variation in fat-free mass hydration can change your DEXA-determined body fat percentage by nearly 3%. This can be a problem when comparing different ethnicities or body types where fat-free mass hydration can vary. It can also be a problem when trying to measure change over time.
DEXA vs. 4-Compartment Models
A number of studies have compared DEXA to 4-compartment models. When looking at group averages, DEXA does pretty well, with errors of 1-2%. However, like with all other body fat testing techniques, individual error rates can be much higher. The error rates vary by what study you look at and which DEXA machine was used; error rates range from 4% in one study to up to 8-10% in another study. Also, the accuracy of DEXA can be affected by sex, size, fatness, and disease state of subjects.
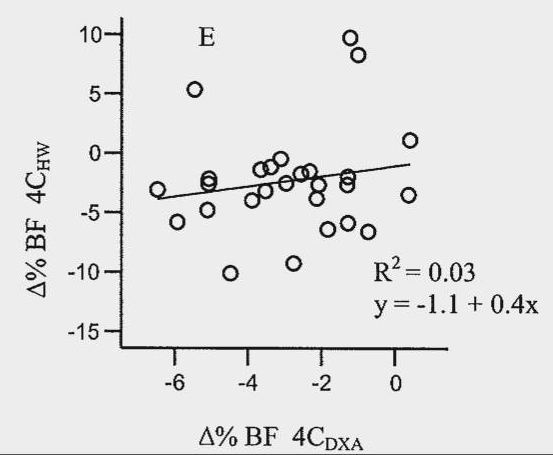
There are also issues when trying to use DEXA for tracking change over time. In one study, researchers wrapped lard around the legs of subjects to simulate weight gain. However, this changed the apparent bone mineral content, questioning the ability of DEXA to accurately assess body composition during weight change. In another study on bodybuilders, DEXA was reasonably accurate when looking at the group change in body fat percentage, but the individual error rate was as high as 4%. Thus, you could decrease your body fat percentage by 4% yet DEXA might show no change, or DEXA might show a 4% change when you didn't really have a change. Another study showed DEXA to overestimate decreases in percent body fat, while it underestimated increases in percent body fat. In fact, the overestimations got as high as 5%. Finally, here's a chart from a study that compared changes in body fat over time using DEXA to using a 4-compartment model:
The X-axis of this chart shows the change in % body fat for DEXA, while the Y-axis shows the change for the 4-compartment model. You can see there was very little agreement between the methods. For example, one person showed an increase in body fat percentage by 5% with the 4-compartment model, but a decrease by 5% according to DEXA. Another person had nearly a 10% loss of body fat according to the 4-compartment model, but only a 3% decrease according to DEXA. These results question the reliability of DEXA for measuring change over time in individuals.
DEXA: The Verdict
Despite the fact that DEXA represents a 3-compartment model, its error rates are no better than hydrostatic weighing, and in some cases is worse. Like other techniques, DEXA does well when looking at group averages, but not so well when looking at individuals. Individual error rates tend to hover around 5%, although some studies have shown error rates as high as 10%. When looking at change over time in individuals, error rates have hovered around 5% in some research, although other research has indicated DEXA to perform much more poorly. For these reasons, I do not recommend DEXA for tracking change over time in individuals. If you do use DEXA for tracking change over time, I recommend very long time periods between measurements (a minimum of 3-6 months), as you will need a minimum of a 5% change in body fat to reliably detect a true change in body fat in most people.
That sums it up for the most widely available techniques for determining body composition. In the final part next week, I will discuss the practical application of everything you have learned in this series.

Thanks for the article. Today I got my first DEXA scan and was very surprised to see a 5% difference in body fat measured on a body impedance scale and DEXA scan. Although overall informative but I can say won’t rely of DEXA scan for measuring body fat. The good old mirror and measuring tape should be enough.
Well written. Good references and consistent w my research on Dexa. The best available option may be whole body MRI for body fat.
Thank you!
A Whole MR for body fat? and does it exist in the Market? Thx
Not of which I’m aware
Hey James, this was a really thorough series and I appreciate all the information about the different methods. I’d been tracking my BF% through DXA, though I am reconsidering on account of the data. I wanted to ask your opinion on this study (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7263310/) which seemed to validate the notion of imitating the “gold standard” 4-component model for BF% by replacing the ADP-Body Volume with a DEXA derived BV measurement, and replacing the Deuterium Dilution Total Body Water with a BIA derived TBW measurement. BV between ADP and DEXA was quite close, but BIA had a larger deviation from D2O.… Read more »
Looks reasonable, although I would’ve liked to have seen some Bland Altman plots to see the limits of agreement and the individual error rates. Also, they removed outliers in their analysis, but in real life, you’re going to have outliers, so it makes me question just how much of a replacement this could be in real world settings.
Hey, what about MRI?
MRI is too difficult/expensive to do for general population, and is better for looking at regional fat. To my knowledge I don’t know if whole body MRI has been validated for assessing overall body fat percentage.
thanks for the content.
one question, though. which is the 4-c model? i imagined it would be the dexa, but it’s not. are you writing something about it?
thanks!
4-compartment model which is described here
Oh my ******* God, it’s all capital letters, automatically! : (
I loved reading these articles! Very informative. How does the navy method for assessing BF% stack versus the methods that you analyzed?
The Navy method is going to be highly inaccurate on an individual level, more inaccurate than these methods
I had a DEXA it said I was up a pound in fat and a pound in muscle since my last one. I feel this is incorrect since I gained 1/2 inches on my arms and lost 2 1/2 inches off my waist.
Well there are a few other body fat measurement techiques not mentioned here namely CT and MRI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3607308/ CT is the most accurate and shown to be 1.3% within cadaveric studies eg they did a CT and measured body fat and then cut all the fat off a dead guy and compared the two. I’d believe the CT was even more accurate as they probably couldn’t cut all the fat off the cadaver without dropping some on their clothes/floor. This makes sense since CT gives a 3d volumetric view of your body with densities of those sections which is easily… Read more »
CT is not practical, cost effective, and there’s the issue with radiation exposure.
DXA is not the normal “gold standard.” Only a 4-C model is the gold standard. The errors go well beyond people not fitting in the machine. I described much of the sources of error in this article (like assumptions about the density of FFM).
5% inaccuracy is good enough for most of us. Who cares if DXA shows 10% body fat and in reality it is 10.5% or 9.5%?!
No, it’s 5 percentage points. So if DXA showed 10%, it could be 5% or 15%.
It is stated as +/- 3% to 5% of fat free mass. Hence measure the ffm Error maximum is 5% of the measured value. Stefan is correct. I assume you do not understand error calculations.
Barry, you are incorrect. Please read the papers I referenced in the article. They are percentage points. I even show a Bland-Altman plot in the article.